技术资料
-
 点播Ancillary Materials Course Learn about the translation pathway for cell and gene therapies, and the ancillary material qualification process.
点播Ancillary Materials Course Learn about the translation pathway for cell and gene therapies, and the ancillary material qualification process. -
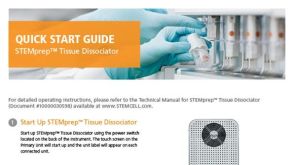
 科学海报Development of Robust T Cell Manufacturing Protocols in Bioreactors Using cGMP-Compliant Ancillary Reagents
科学海报Development of Robust T Cell Manufacturing Protocols in Bioreactors Using cGMP-Compliant Ancillary ReagentsConference:
ISCT 2025
 EasySep™小鼠TIL(CD45)正选试剂盒
EasySep™小鼠TIL(CD45)正选试剂盒













 沪公网安备31010102008431号
沪公网安备31010102008431号