技术资料
-
 挂图Regulatory T Cells Overview of the development, phenotype and functions of regulatory T cells
挂图Regulatory T Cells Overview of the development, phenotype and functions of regulatory T cells -
 挂图The Immune Response to HIV Poster Summary of how HIV subverts the immune response to establish a chronic infection
挂图The Immune Response to HIV Poster Summary of how HIV subverts the immune response to establish a chronic infection -
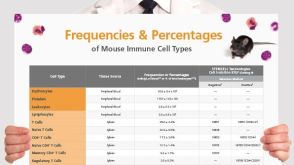 挂图Frequencies and Percentages of Mouse Immune Cell Types List of the frequencies of over 25 immune cell types in C57BL/6 mice
挂图Frequencies and Percentages of Mouse Immune Cell Types List of the frequencies of over 25 immune cell types in C57BL/6 mice -
 挂图Antigen Processing and Presentation Overview of the mechanisms by which antigens are processed and presented to T cells
挂图Antigen Processing and Presentation Overview of the mechanisms by which antigens are processed and presented to T cells -
 挂图Frequencies of Human Cell Types in Blood-Related Sources List of the frequencies of over 35 cell types in normal human blood-related sources.
挂图Frequencies of Human Cell Types in Blood-Related Sources List of the frequencies of over 35 cell types in normal human blood-related sources.


 EasySep™小鼠TIL(CD45)正选试剂盒
EasySep™小鼠TIL(CD45)正选试剂盒












 沪公网安备31010102008431号
沪公网安备31010102008431号