技术资料
-
 技术公告StemSpan™ Medium and Supplements for the Generation of T Cells from Cord Blood-Derived CD34+ Cells
技术公告StemSpan™ Medium and Supplements for the Generation of T Cells from Cord Blood-Derived CD34+ Cells细胞类型:
T 细胞,造血干/祖细胞,CD4+T细胞,CD8+T细胞
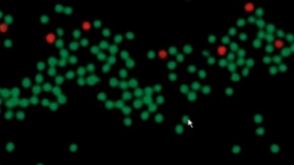
 EasySep™小鼠TIL(CD45)正选试剂盒
EasySep™小鼠TIL(CD45)正选试剂盒















 沪公网安备31010102008431号
沪公网安备31010102008431号